Becoming a Physician in the Time of COVID-19: Big Dreams and Doing Things Differently
With a penchant for people, anatomy, and the heart, Dr. Jennaire Lewars navigates the transition between medical school and residency in the midst of COVID-19, and shares his plan to help underserved communities.
by Dr. Jennaire Lewars and Victoria Oldridge
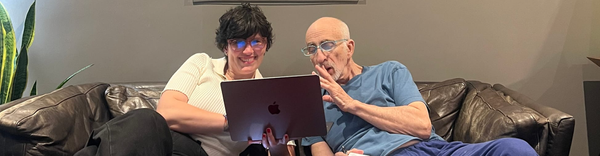
Dr. Jennaire Lewars is an Internal Medicine Resident at Carle Foundation Hospital in Illinois. Originally born in Jamaica, Dr. Lewars immigrated to Toronto, Canada in early childhood.
Truffld: As fields of study have broadened exponentially in the last decade, making it difficult for some college-bound students to decide on a path, applications to medical school continue to increase at a steady rate of 3% per year – even higher during the onset of COVID-19. What led you toward medicine, and specifically, cardiology?
Dr. Lewars: Education has always been a fundamental component of my upbringing, especially coming from a Jamaican family, so the importance of my educational pursuits have always been reinforced. My dad is an accountant who owns a small business and my mother is a registered nurse. Regarding my interest in medicine, while my mother was in nursing school, she handed me one of her anatomy books to delve into over the summer holiday when I was 12 years old. She said "Just choose an organ system and learn about it, be productive." I chose the heart which sparked my intrigue in medicine. I chose to learn its anatomy, became fascinated with it and even practiced sketching it, as I'm a sketch artist by hobby. As I matured, my interest in the heart and cardiology heightened, primarily due to comorbidities like hypertension and diabetes that I witnessed plaguing my own family. Over time I developed a yearning for change, to help those suffering from cardiac ailments, to impart my own experience and also apply my love for people and humanity in patient care settings. Also, seeing the impact of heart disease in my community, the lack of resources, access to healthy foods and quality health care and the holistically deplorable effect of these factors on the minority population invoked a desire to be an advocate for my community and beyond.
Truffld: You're quite active on social media and you're really leveraging it for positivity, not only to shine a light on the rise of other Black men and women going into medicine, but also to inform.
Dr. Lewars: When you look at the overall numbers for African Americans in clinical roles, they're still very low, but when I post something on Instagram and we all cross-tag one another and bring attention toward each other's journeys, we can see our global impact and start to realize just how much more our community is growing in this field.
My overarching tones on social media have been to let others know that they can accomplish this [becoming a physician] as well. Even though I am aware that not everyone is afforded the same opportunities that I may have had, knowing my own struggles to reach this point such growing up as a minority, and an immigrant from an inner city community that lacked access to much, I want to implore others to pursue their dreams whatever they may be. I strive to motivate others to do more in this world, and to know that no matter our backgrounds, we can do great things.
During medical school, I made note of the amount of diversity in my surroundings throughout my training. To some degree early on there was quite a bit of diversity, but once I entered the clinical arena, I found that there was much less so from the standpoint of Attending Physicians, practitioners and even nursing staff overseeing my training during some rotations. In that regard it was a bit challenging not seeing others like myself with similar experiences and viewpoints on the world as it applied to my medical foundation but this did assist in my training because it enabled me to adapt and mold. Diversity in medicine is important with respect to looking at a patient population – specifically a minority population, and it's imperative to have that [background] identification with your patient. More importantly, inherent bias isn't as prominent when you're able to share commonalities, and additionally, the effort to delve beyond stereotypes and stigmas, which facilitates treatment.
As for becoming a doctor as a minority, many people can't see the path forward nor believe in the possibility of their potential, especially if they hadn't ever seen a Black doctor or even specialists growing up, as I hadn't. However, when others see examples of such – those who are innovators and changing the scope of medicine -- along with receiving guidance and developing the ability to seek out opportunities and resources, this path becomes much more visible and the dream becomes tangible.
Truffld: Graduate school or even undergraduate school can feel daunting for some, and you make it look easy. How is that?
Dr. Lewars: My life experiences have caused me to develop a great degree of resilience. I got into medicine without a plan B; this is what I have always wanted to pursue. There were a lot of junctures where it felt really difficult, but at no time did I not know that it was worth it. I have a lot of people counting on my success, and for that I have no choice but to apply my best efforts no matter what my circumstances are. It isn’t an easy feat, but it’s also all in the pursuit of a career that I love, so my pleasure and enjoyment in this journey may make it appear easy as I embrace the process.
Some of the toughest instances for me were times of financial difficulty during my training. Finances are a hurdle for a lot of people when it comes to education. During medical school I learned that I needed to cultivate some ingenuity to get around these hurdles such as learning how to adequately manage my money, ration my food, and to be disciplined with my budget.
I believe that we don’t have to wholly rely on others [on an institution] to provide or supplement our needs. We need to be innovative. In medical school there were certain resources we didn't have on campus, so we created them – I realized that there were aspects of clinical training that we needed more of, so my colleagues and I formed a fraternity that allowed us to plug into the community more, perform health screenings, produce extra-curricular training and more. Sometimes, you have to make things work for yourself to make it.
Truffld: The last year of medical school for you was during the onset of COVID-19. How did that impact your curriculum?
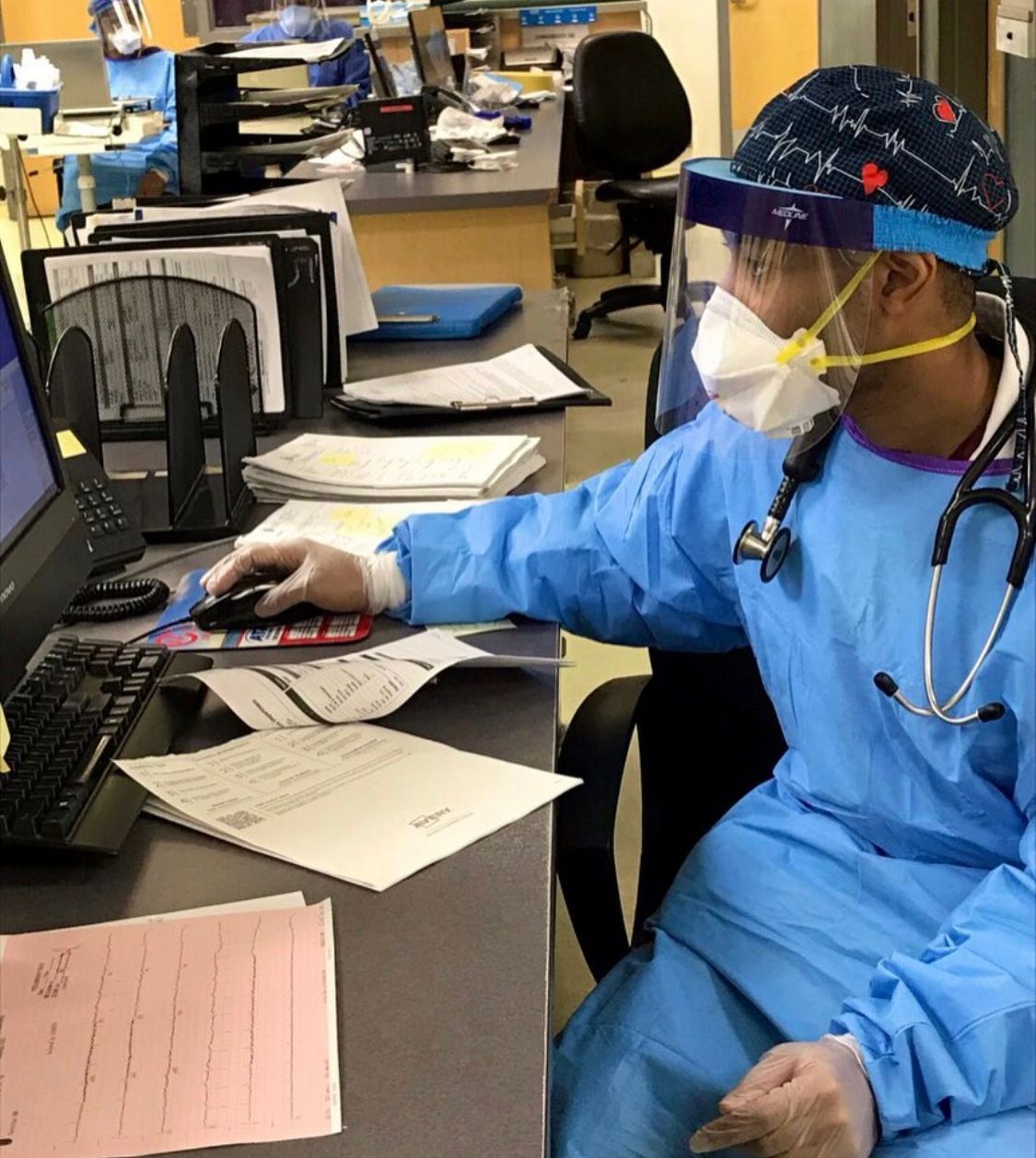
Dr. Lewars: Right before I graduated, I had a few more rotations left, but they were cancelled as this was within the initial peak of the pandemic. I had a strong desire to still be a part of the front line force working their way to help so many people suffering from this virus. I was amongst one of the first sets of medical students in the Chicago area who chose to volunteer in the community as I decided to assist within a packed emergency department on the South Side of Chicago. Though I was no longer in rotation, I was able to still hone my educational experiences and learn a lot in the process.
Our professors have continued to send us the most current COVID data and guidelines. To some regard, we were more informed about COVID before the general public, though information on its spread and severity were not well developed at that point. In a crisis that hinges so much on the need for reliable data and communication, the impact of opinions, and information spread on health outcomes has heightened. When it comes to media coverage, stories and assumptions about this pandemic [and more] can quickly become sensationalized or politicized. Not everyone in the media has a medical background, so it's up to us as medical professionals to rectify certain things that may induce misinformation. With that said, I encourage people to be proactive in informing themselves, seek reliable sources of insight, and be diligent in the pursuit of their own health knowledge.
This week there were a number of anti-vaxxers on social media who were commenting on my page to a harassing degree, imposing their viewpoint on the pandemic. I tell people that our job is to provide the information that we have accurately and holistically, not to force you into something. If you have a different ideology, that's your choice. Once again I encourage everyone to utilize their autonomy but be well informed and unbiased while doing so.
Truffld: Conventional, western medicine can be very focused on palliative (symptomatic) treatment, but not holistic, total systems care. When many clinicians have only 8 minutes to spend with each patient, we're oftentimes putting 'band-aids' on the issue, rather than treating sustainably and systemically.
Dr. Lewars: Yes, and I'd like to take a different approach – it's one of the reasons I'm even establishing a social media base because I want to be able to leverage these tools to teach people about how to govern their health, signs to pay attention to, and affordable nutrition that will enable them to thrive. Patient education, I believe, is a cornerstone of clinical practice – even holding basic knowledge of diseases and ways to prevent them can reduce the healthcare burdens that we face, and result in better and more sustainable outcomes as a whole. This information will proliferate a community and have generational impact. There's a lot I want to do – from opening health centers to supporting scholarship programs, and helping underserved populations – so that comprehensive healthcare is accessible to everyone.
Follow Dr. Jennaire Lewars on IG